County, university combine for 19 new cases
Published 6:08 pm Thursday, August 20, 2020
|
Getting your Trinity Audio player ready...
|
Pike County added 13 cases of COVID-19 overnight Wednesday.
The new cases bring the county’s total to 753 with seven confirmed deaths.
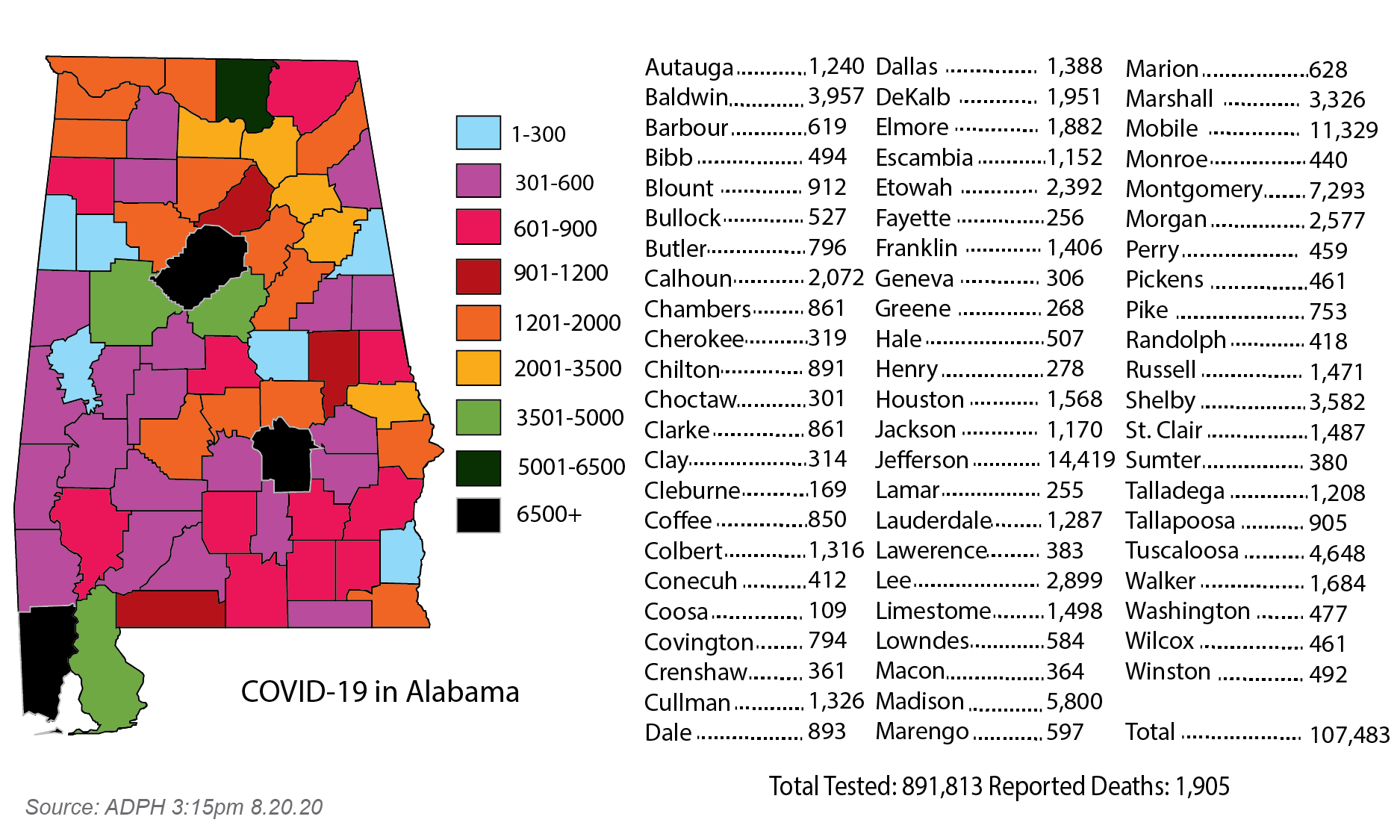
Statewide, only 699 new cases were reported in the Alabama Department of Public Health 10 a.m. update, bringing the total to 107,483.
Despite rises in some areas, the overall state daily case rate continues to decline since mid-July, when Gov. Kay Ivey announced a statewide mask mandate. In the week before the mandate, the 7-day average for new cases was 1,652; last week, it was 855.
Pike County remains in the “high risk” category according to the ADPH, with its 7-day average for new cases at 5.29.
In addition to the ADPH case count, Troy University reported 10 new cases of coronavirus on Thursday, including a fourth in one residence hall.
The cases reported include eight off-campus students, one at Farmhouse Fraternity and one in Rushing Hall, which now has four confirmed cases. Both Trojan Village and Delta Chi Fraternity have reported two cases.
Because the ADPH records cases based on the county of home residence, most of the Troy cases are not included the ADPH count for Pike County.
The university has self-reported 60 cases among students, including 13 on campus, since students returned on Aug. 10 and five among employees.
As more is learned about COVID-19, the Alabama Department of Public Health (ADPH) is providing updated guidance about testing priorities, listing and defining types of tests, and quarantine and isolation requirements for COVID-19 patients and their contacts.
No one is immune to COVID-19, but it impacts some populations and communities disproportionately, the ADPH said in a statement.
Everyone has a responsibility to help slow the spread of the virus in their homes, workplaces, educational institutions and other places within their communities. Because COVID-19 testing resources are not sufficient to test every person at this time, ADPH recommends the following guidance in a health alert network message to providers.
Testing priorities for patients and laboratories:
1. Hospitalized individuals with signs or symptoms of COVID-19 infection.
2. Other symptomatic individuals and higher risk asymptomatic individuals including but not limited to those in long-term care facilities.
3. Other individuals not experiencing symptoms when certain conditions exist.
Types of tests:
1. Diagnostic tests assess the presence of the virus at a given point in time. A negative means only that an individual was negative at the time of the test. This can be impacted by factors including but not limited to the quality of the specimen collected, the timing of collection during the incubation period, and the handling of the specimen.
2. Polymerase Chain Reaction (PCR) tests and Nucleic Acid Amplification testing (also known as viral tests) detect the RNA genetic material in the COVID-19 virus and are often collected via nasal pharyngeal, mid turbinate, nasal, oral or throat swab or saliva collection. Some of these tests are now available at the point of care.
3. Antigen tests detect the presence of COVID-19 specific protein particles and are collected via a respiratory sample. Currently, two approved point-of-care tests are being utilized.
4. Serology (antibody) tests are not diagnostic tests. These tests detect antibodies in the blood indicating possible prior exposure to COVID-19 which may develop 6-14 days after infection. Commercially available antibody tests have variable performance.
Isolation, quarantine and employer requirements about returning to work and retesting:
1. At the time of testing, persons are instructed to isolate at home while awaiting test results. Persons who are close contacts to COVID-19 cases must complete at least a 14-day quarantine period even with a negative test.
2. Individuals who test positive for COVID-19 should isolate from others in the home to reduce the risk of spread. If those who test positive cannot isolate from household members, then household members must remain in home quarantine 14 days after the person who tested positive is released from isolation.
3. Employers should not routinely require a negative laboratory COVID-19 test as a requirement for employees to return to work. This is because PCR tests can remain positive long after an individual is no longer infectious. Instead, symptom- or time-based methods are recommended with some very rare exceptions. However, this does not mean an employer must allow an employee who currently has COVID-19 to return to work before the employee’s infection is resolved.
4. Persons who tested positive for COVID-19 and have recovered do not need to be quarantined again or be re-tested for at least 90 days unless they develop new symptoms consistent with COVID-19 infection.
Close contacts and when to leave quarantine:
1. A close contact is anyone who has known exposure defined as being within 6 feet of a COVID-19 infected person for 15 minutes or greater within a 24-hour period. The 15-minute time is a cumulative period of time. For example, a close contact might be within 6 feet of a COVID-19 positive person for 5 minutes each at 8 a.m., noon and 5 p.m. This is a standard based on guidance from the CDC.
2. A person who is a close contact to a confirmed or probable COVID-19 case must complete at least a 14-day quarantine period, regardless of whether a face covering, or regular mask was worn.
3. Persons with known exposure who are determined to meet the close contact definition cannot leave quarantine, regardless of whether they test negative for COVID-19. This means that a negative COVID-19 test will not allow them to return to work, school or participate in sports or other activities. This is because a person who has been exposed to COVID-19 and meets the close contact definition has up to 14 days to become infected from the time of exposure. This period may be even longer for a small number of people.
4. Allowances regarding close contacts are made for healthcare personnel who wore the appropriate personal protective equipment.
For more information about COVID-19, go to alabamapublichealth.gov.